(Last Update: 11/14/2024)
This content is created with integrity and impartiality; we do not receive direct compensation for this review. See our Mission and Core Values here.
Welcome to "Sleep Apnea Secondary to Tinnitus: Strategies for Relief," where we delve into the intricate, causal connection between tinnitus and sleep apnea and its profound impact on individuals' lives.
This post aims to show how these conditions intertwine, leading to sleep disturbances and reduced quality of life.
We will explore effective strategies and innovative solutions to manage and alleviate symptoms, offering hope and guidance to those navigating the challenges of living with tinnitus-induced sleep apnea.
What Is Sleep Apnea Secondary to Tinnitus?
When sleep apnea occurs as a severe secondary condition to tinnitus, it presents a unique challenge in identification and management. Understanding the interplay between the severity of these two conditions is crucial for those seeking relief and returning to restful nights.

Obstructive Sleep Apnea (OSA)
Characterized by airway blockages during sleep, OSA is the most common form. The Obstructive Sleep Apnea Syndrome is a sleep disorder where airway blockages cause breathing pauses, disrupting sleep and lowering oxygen levels, leading to daytime fatigue.
Central Sleep Apnea (CSA)
CSA involves the brain failing to signal muscles to breathe.
Complex Sleep Apnea Syndrome
This form combines OSA and CSA symptoms.
When these types of sleep apnea occur as secondary conditions to severe tinnitus, diagnosing and managing them becomes complex. The interplay between sleep apnea and tinnitus necessitates a comprehensive approach to treatment.
What is Tinnitus?
Tinnitus is characterized by hearing and other noises, like ringing, buzzing, or humming, in the ears when no external sound is present. It can result from various causes, including exposure to loud noise, ear infections, or age-related hearing loss.
Common Symptoms and Signs
Nighttime Symptoms
Individuals suffering from sleep apnea secondary to tinnitus often report a distinct set of nighttime symptoms. These include disrupted sleep due to frequent awakenings from loud noises, a direct result of the intrusive nature of tinnitus sounds.
Moreover, typical sleep apnea symptoms such as loud snoring, gasping for air, or experiencing breathing pauses are common.
The co-occurrence of one study of these tinnitus symptoms can significantly impact sleep efficiency, making it difficult to achieve deep, restorative rest.
Daytime Effects
The daytime effects of sleep apnea are multifaceted, affecting both physical and mental well-being. Chronic fatigue is a predominant complaint stemming from poor sleep quality.
This fatigue can exacerbate the perception of tinnitus and daytime fatigue, creating a vicious cycle.
Diagnosis: Connecting Tinnitus with Sleep Apnea
Clinical Evaluation
Diagnosing sleep disturbance secondary to tinnitus involves a comprehensive clinical evaluation.
Healthcare providers will often conduct a thorough history and physical examination, paying close attention to the patient's sleep patterns, daytime symptoms, and the specific characteristics of their tinnitus.
This evaluation may include discussing secondary conditions in the patient's medical history and focusing on factors contributing to or exacerbating both conditions.
Specialized Testing of Related Diseases
Specialized testing plays a pivotal role in connecting tinnitus with sleep apnea. A polysomnogram, or sleep study, is commonly used to diagnose sleep apnea by monitoring various physiological parameters during sleep. Audiological exams may also be conducted to assess the severity and impact of tinnitus.
Sleep apnea is related to oxygen levels. It is a condition in which breathing frequently stops and starts during sleep, leading to decreased oxygen levels in the blood. This oxygen reduction can have various health implications, including increased risk for cardiovascular disease.
Combined with the clinical evaluation, these tests can help healthcare providers determine how much tinnitus contributes to sleep apnea service other disturbances and tailor a treatment plan that effectively addresses both conditions.
How does sleep apnea secondary to tinnitus Affect Military Veterans?
VA Disability Claims
Many veterans grappling with sleep apnea secondary to tinnitus encounter significant hurdles when navigating VA disability claims. The claim process requires thorough documentation to establish the health issues as service-connected, a step vital for a veteran to secure the deserved recognition and support.
Service Connection and VA Benefits
Successfully proving a secondary service connection for sleep apnea related to tinnitus can substantially impact a veteran's VA disability rating.
What is a VA disability rating? It is a percentage of military personnel with extensive experience assigned to a veteran's service-connected injury or illness, determining compensation levels.
This determination of VA rating is critical, as it directly influences access to VA benefits, which provide much-needed assistance in addressing health challenges after serving their country.
Veterans Health Complications :
For veterans, high blood pressure often complicates the already difficult journey of managing sleep apnea secondary to tinnitus. Recognizing and treating these conditions as interconnected is essential for improving veterans' quality of life, underscoring the need for comprehensive healthcare solutions that address the full spectrum of service-related health issues.
While Tinnitus may not cause hearing loss, it is often a symptom of an underlying condition that may affect hearing. It is characterized by hearing noises like ringing, buzzing, or humming in the ears when no external sound is present.
Identifying this sleep apnea requires a nuanced understanding of both conditions and a tailored approach to diagnosis and treatment.
Recognizing the common tinnitus symptoms and signs of secondary conditions and undergoing a thorough diagnosis is essential to managing these intertwined health challenges and improving overall well-being.
Heart disease, insulin resistance, and blood flow issues are related to tinnitus and sleep apnea. Poor cardiovascular health worsens tinnitus through altered blood flow, while sleep apnea, linked to heart disease, can stress the heart. Insulin resistance, associated with obesity, connects to sleep apnea and indirectly to tinnitus via metabolic health.

Strategies for Managing Tinnitus-Induced Sleep Apnea
Dealing with sleep apnea influenced or exacerbated by tinnitus requires a strategic approach to mitigate symptoms and improve sleep efficiency.
Lifestyle Adjustments for Improved Sleep
Optimizing the Bedroom Environment
- Sound Masking: Utilize white noise machines or apps to mask the ringing of tinnitus, which can help distract the brain and facilitate easier sleep onset.
- Comfort and Calm: Ensure the bedroom is cool, dark, and quiet. Investing in comfortable bedding and minimizing light exposure can significantly impact sleep quality.
Health and Dietary Considerations
- Avoid Stimulants: Reduce consumption of caffeine and alcohol, particularly in the hours leading up to bedtime, as they can exacerbate tinnitus and disrupt sleep patterns.
- Regular Exercise: Consistent physical activity can improve overall sleep quality and reduce the intensity of sleep apnea symptoms. However, avoid strenuous workouts close to bedtime as they might energize rather than relax.
Behavioral Therapies: Mindfulness and Relaxation Techniques
Mindfulness Meditation
- Stress Reduction: Mindfulness meditation can reduce stress levels, often exacerbating tinnitus and sleep apnea symptoms. By focusing on the present and employing deep breathing techniques, individuals can achieve a state of calm before bedtime.
- Routine Implementation: Incorporating a short meditation session into the nightly routine can signal to the body that it’s time to wind down, preparing the mind for sleep.
Relaxation Techniques
- Progressive Muscle Relaxation (PMR): PMR involves tensing and slowly relaxing different muscle groups. This practice can ease the physical tension that might contribute to difficulty falling asleep.
- Guided Imagery: Listening to guided imagery or relaxation scripts can divert attention from tinnitus sounds and induce sleepiness.
Managing tinnitus-induced sleep apnea involves practical lifestyle changes and behavioral therapies to enhance relaxation and sleep readiness.
Medical Interventions for Relief
Navigating the challenges of sleep apnea, especially when compounded by tinnitus, requires a multifaceted treatment approach.
Medical interventions offer significant relief, with options ranging from CPAP therapy to alternative treatments like oral appliances and surgery.
Understanding these options can guide sufferers toward making informed decisions that enhance their sleep efficiency and life.
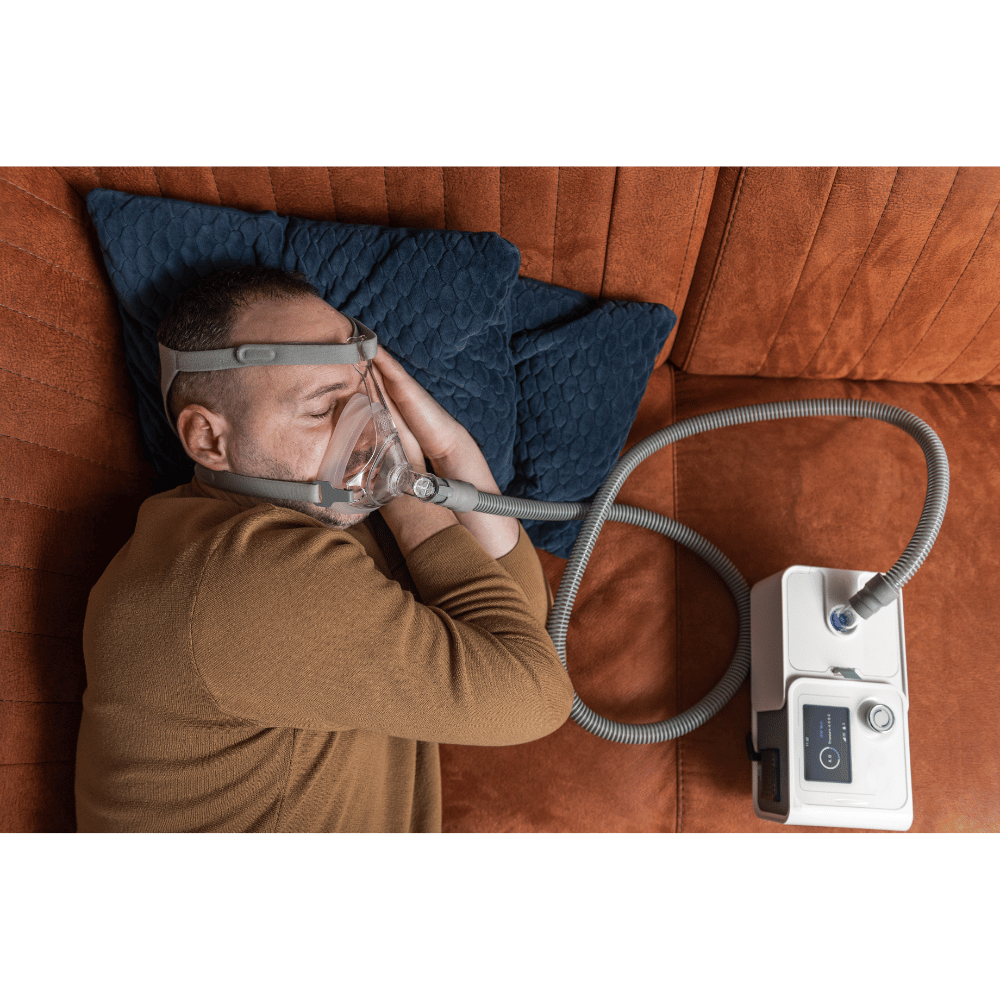
CPAP Therapy: Adapting for Tinnitus Sufferers
Customizing CPAP Settings
- Adjustable Pressure Settings: Tinnitus sufferers can benefit from a CPAP machine that allows for personalized pressure settings, ensuring comfort while effectively keeping the airway open.
- Sound-Masking Features: Some CPAP devices come with built-in white noise generators or allow for external sound therapy devices to be connected, helping mask tinnitus sounds and facilitate easier sleep.
Sleep Disturbances: Enhancing Comfort with CPAP Accessories
- Comfortable Masks: Selecting a CPAP mask that fits well and is comfortable can reduce the potential for additional sleep disturbances, making it easier for tinnitus sufferers to adapt to the therapy.
- Humidifiers: Adding a humidifier to the CPAP setup can prevent dryness and irritation in the airway, addressing a common complaint among CPAP users and potentially easing tinnitus symptoms.
Alternative Treatments: Oral Appliances and Surgery Options
Oral Appliances for Sleep Apnea
- Mandibular Advancement Devices (MADs): These devices gently push the lower jaw forward, enlarging the airway and reducing sleep apnea symptoms. For those with tinnitus, MADs can offer a quieter, more comfortable alternative to CPAP therapy.
- Tongue-Retaining Devices (TRDs): TRDs hold the tongue in place to keep the airway open. They are less intrusive and can be easier for some sleep apnea patients patients to tolerate.
Surgical Interventions
- Uvulopalatopharyngoplasty (UPPP) removes excess tissue from the throat, widening the airway. It's suited for patients with obstructive sleep apnea whose tinnitus may be exacerbated by apneic events.
- Inspire Therapy: A more recent advancement, Inspire Therapy consists of the surgical implantation of a device that stimulates the nerves controlling the tongue and airway muscles, keeping the airway open.
Innovative Therapies and Emerging Research
The treatment landscape for conditions like tinnitus and sleep apnea is ever-evolving, with innovative therapies and groundbreaking research leading the charge toward more effective and less invasive solutions.
These advancements promise a future where managing these conditions could become significant.
Sound Therapy for Tinnitus and Sleep Apnea
Utilizing White Noise and Sound Masking
Sound therapy has emerged as a cornerstone in treating tinnitus, utilizing white noise or specific frequencies to mask the intrusive sounds experienced by sufferers.
This approach has also shown promise for individuals with sleep apnea, as certain sounds can promote relaxation and ease the transition into deeper sleep stages, indirectly benefiting those with sleep disturbance caused by tinnitus.
The Future of Treatment: Technological Advances
Wearable Technology and Monitoring Devices
Integrating wearable technology into managing sleep apnea and many other conditions in tinnitus patients represents a significant leap forward.
Devices that monitor sleep patterns, sleep-disordered breathing, and even heart rate offer real-time data that can adjust treatment plans dynamically.
Gene Therapy and Molecular Medicine
At the forefront of emerging research is exploring gene therapy and molecular medicine as potential cures for tinnitus and sleep apnea.
Though still in the early stages, this research holds the promise of fundamentally changing the approach to treatment, moving from symptom management with medications to actual cures.
Personal Management: Tips from the Community
Living with tinnitus-induced sleep apnea can be challenging, but personal management strategies developed through community wisdom offer practical ways to mitigate symptoms and improve quality of life.
Daily Routines for Managing Symptoms
Establishing a Consistent Sleep Schedule
Creating a consistent sleep routine is essential to the cornerstone tips shared by individuals who have navigated the complexities of tinnitus and sleep apnea.
Going to bed and waking up at the same time daily helps regulate the body's internal clock, improving sleep quality over time.
Creating a Pre-Sleep Ritual
Another widely recommended strategy involves creating a calming pre-sleep ritual to signal the body that it's time to wind down.
This can include reading, taking a warm bath, or practicing relaxation techniques. For individuals with chronic tinnitus, however, incorporating sound therapy into this ritual — such as listening to white noise and nature sounds — can help mask tinnitus sounds and facilitate the transition to sleep.
Embracing a Holistic Approach
Many success stories emphasize the importance of a holistic approach to managing symptoms, incorporating physical and mental health strategies.
By addressing the broader spectrum of health, individuals often find they can better manage their symptoms and improve their overall well-being.
Personal management tips from the community offer invaluable insights for those dealing with tinnitus-induced sleep apnea.
Navigating Challenges: Mental Health and Coping Mechanisms
Living with conditions like tinnitus-induced sleep apnea and hypertension can pose significant challenges not only to physical health but also to mental well-being.
The Psychological Impact of Chronic Conditions
Anxiety and Depression
- Increased Risk: Individuals with chronic conditions like tinnitus and sleep apnea may experience higher rates of anxiety and depression due to the persistent discomfort and sleep disturbances they cause.
- Feedback Loop: The stress from these mental health challenges can, in turn, exacerbate the symptoms of the physical conditions, creating a challenging cycle of worsening mental and physical health.
Impact on Daily Life
- Social Withdrawal: The constant battle with sleep deprivation and the intrusive nature of chronic tinnitus can lead to withdrawal from social activities, as individuals may feel misunderstood or unable to participate fully in life.
- Professional and Personal Strain: Difficulty concentrating, fatigue, and irritability can strain professional relationships and personal connections, further impacting an individual's quality of life.
Support Systems and Seeking Help
Building a Support Network
- Community Groups: Engaging with online forums or local support groups for those with sleep disorders related to tinnitus or sleep apnea can provide a sense of community and understanding, offering practical advice and emotional support.
- Family and Friends: Educating close family members and friends about the conditions can help them understand the challenges, enabling them to offer more meaningful support and accommodation.
Professional Mental Health Support for Sleep Problems
- Counseling and Therapy: Seeking professional help from therapists or counselors who specialize in chronic conditions can equip individuals with strategies to manage anxiety, depression, and stress related to their health issues.
- Medical Intervention: In cases where mental health and sleep disorder significantly deteriorates, consulting with healthcare professionals for potential medication or targeted therapies can be crucial in maintaining mental well-being.
CONCLUSION:
Navigating the challenges of sleep apnea secondary to tinnitus requires a multifaceted approach, blending lifestyle changes, medical interventions, and mental health support.
We've explored various strategies that promise improved sleep and health, emphasizing the importance of personalized care and resilience.
As you continue to manage these conditions, remember that progress is possible, and relief is within reach. Stay encouraged, seek support, and embrace each step toward a restful night and a healthier life.
Frequently Asked Questions
What is service-connected tinnitus?
Service-connected tinnitus is recognized by the Department of Veterans Affairs (VA) as linked to military service, making veterans eligible for compensation and healthcare. It requires evidence of the condition arising or worsening due to service duties, establishing a direct connection to their time in the military.
Which one is related to weight gain, tinnitus, or sleep apnea?
Sleep apnea is more directly related to weight gain. Obesity is a serious risk for sleep apnea, as excess weight, especially around the neck, may obstruct the airway during sleep, leading to the condition. Weight gain can exacerbate sleep apnea or increase the risk of developing it.