Last Update: 02/28/2025)
This content is created with integrity and impartiality; we do not receive direct compensation for this review. See our Mission and Core Values here.
Obstructive Sleep Apnea ICD-10: Diagnosis & Treatment Options
Obstructive Sleep Apnea (OSA), classified under ICD-10, presents a significant health concern worldwide.
Characterized by recurrent airway collapse during sleep, OSA disrupts normal breathing patterns, leading to fragmented sleep and diminished oxygen levels.
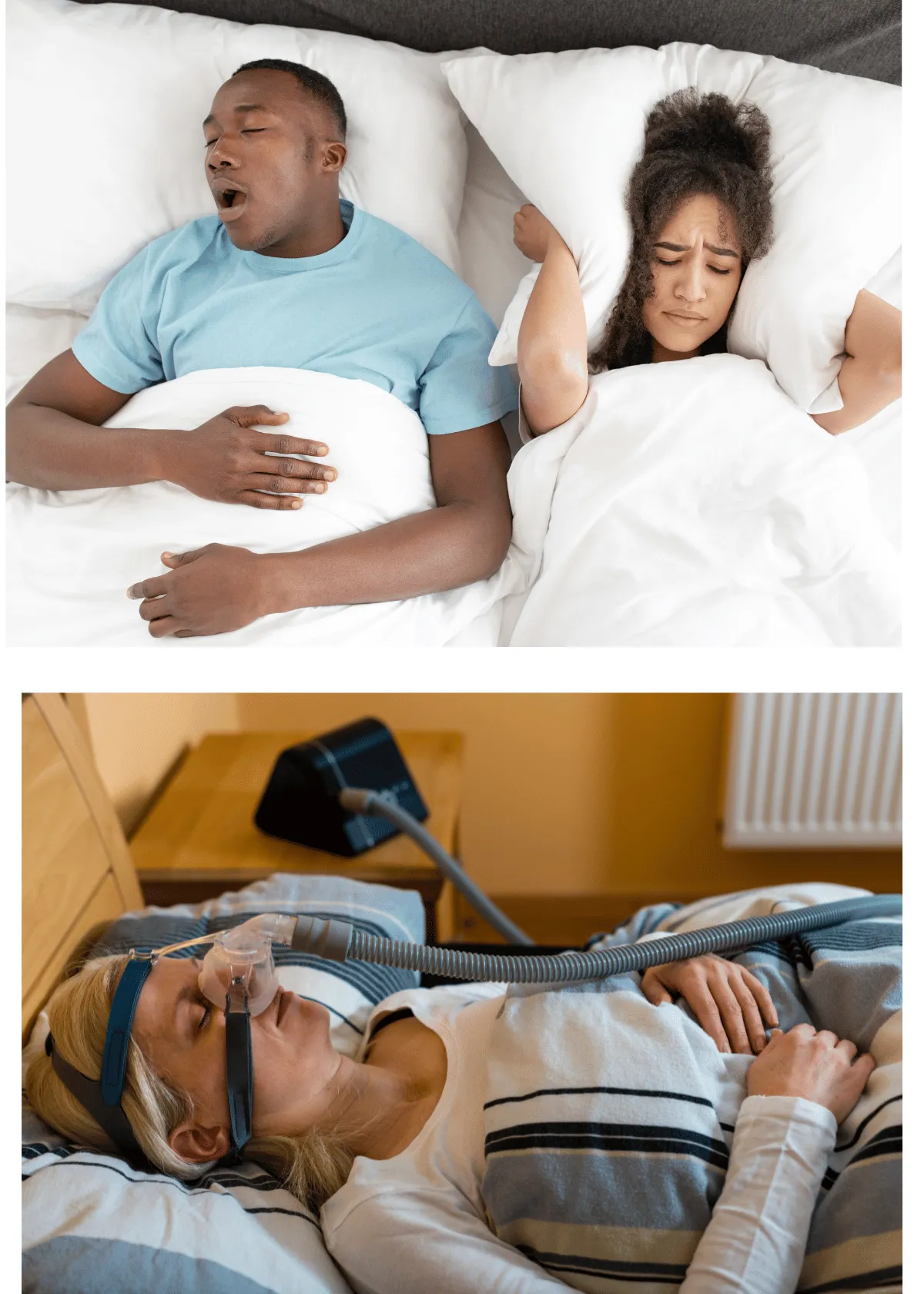
Typical symptoms include loud snoring, daytime fatigue, and morning headaches. Left untreated, OSA increases the risk of hypertension, heart disease, and stroke.
This guide explores various treatment options for managing adult OSA effectively. It emphasizes the importance of early detection and intervention for improving quality of life and overall health.
Understanding Sleep Apnea and Its Impacts
Sleep apnea is a common sleep disorder characterized by repeated interruptions in breathing during sleep. These interruptions occur when the throat muscles relax excessively, causing airway obstruction. In cases of moderate to severe OSA (obstructive sleep apnea), this leads to significant oxygen deprivation, disrupting the ability to fall asleep peacefully and stay asleep throughout the night.
While mild forms of sleep apnea can result in symptoms like snoring and fatigue, moderate to severe OSA poses more serious health risks. Prolonged oxygen deprivation can lead to complications such as coronary artery disease, irregular heartbeat, and other cardiovascular conditions.
Conditions like upper airway resistance syndrome, a less severe form of airway obstruction, can progress into OSA if left untreated, further impacting sleep quality and overall health. Recognizing and addressing sleep apnea is crucial to mitigating these risks and improving sleep health.
Diagnosis of Obstructive Sleep Apnea Adult
Recognizing Sleep Apnea Symptoms and Risk Factors
Obstructive Sleep Apnea (adult/pediatric)is a sleep disorder manifesting through various symptoms and risk factors. Patients often report excessive daytime sleepiness, loud snoring, and incidents of breathing cessation during sleep.
Additionally, individuals with OSA might experience morning headaches, dry mouth, and irritability. Obesity, advanced age, male gender, and anatomical abnormalities such as inflamed tonsils or a recessed jaw increase the risk of developing OSA.

Pediatric obstructive sleep apnea vs. adult obstructive sleep apnea?
Obstructive sleep apnea (OSA) affects both children and adults, but its presentation, underlying causes, and associated conditions vary significantly between these groups. Understanding these differences is crucial for accurate diagnosis and effective treatment.
Pediatric Obstructive Sleep Apnea
Obstructive Sleep Apnea (ICD-10 code G47.33) occurs when the muscles in the throat relax excessively during sleep, leading to airway blockage. As a result, breathing stops momentarily, sometimes for several seconds, causing sleep disruptions and oxygen deprivation.
Pediatric OSA is characterized by recurrent apneas and persistent respiratory effort during sleep, leading to sleep disordered breathing patterns. It is often associated with anatomical or developmental factors such as enlarged tonsils, adenoids, or craniofacial abnormalities. Obesity can also contribute to OSA in children, increasing airway obstruction risk.
Children with OSA may exhibit symptoms such as:
- Daytime tiredness despite adequate sleep duration.
- Behavioral issues like hyperactivity, inattention, or mood swings, often mimicking conditions such as ADHD.
- Disturbed sleep patterns, including frequent awakenings, gasping, or snoring.
In newborns, sleep apnoea is a concern, especially when linked to underlying conditions like prematurity or congenital abnormalities. Recurrent apneas in infants can lead to poor oxygenation, impacting growth and development.
Adult obstructive sleep apnea syndrome
In adults, OSA is typically associated with obesity and related health issues. The condition is marked by repeated airway obstruction during sleep, leading to fragmented sleep and poor oxygenation. Adult OSA is often linked to comorbidities like Pickwickian syndrome, a condition characterized by obesity-related hypoventilation during sleep.
Common symptoms in adults include:
- Loud, habitual snoring often noticed by partners or family members.
- Daytime fatigue and reduced cognitive function, such as difficulty concentrating or memory problems.
- Circadian rhythm sleep disturbances, including altered sleep-wake cycles.
Adult OSA may also lead to more severe complications, including elevated pulmonary arterial pressures. Repeated airway obstruction causes fluctuations in these pressures, increasing the risk of cardiovascular complications such as hypertension and heart failure.
Night terrors and other parasomnias are occasionally observed in adults with OSA, further disrupting sleep and contributing to poor overall sleep quality. Additionally, Cheyne-Stokes breathing, a distinct pattern of breathing characterized by cycles of deep breaths followed by apnea, is more common in adults, particularly those with conditions like congestive heart failure, stroke, or brain injury.
Differences in Underlying Causes
The causes of OSA differ significantly between pediatric and adult populations:
- Pediatric OSA is predominantly caused by anatomical factors like enlarged tonsils or adenoids, which physically block the airway. Other contributing factors include craniofacial abnormalities or obesity in older children.
- Adult OSA is closely tied to lifestyle factors such as obesity, alcohol use, and smoking, along with aging-related decreases in muscle tone in the airway.
Pulmonary Arterial Pressure in OSA
In both children and adults, OSA can lead to increased pulmonary arterial pressures. However, the effects are more pronounced in adults due to prolonged exposure to repeated apneas over time. This fluctuation in pressures during sleep places additional strain on the cardiovascular system, elevating the risk of long-term health complications.
Cheyne-Stokes Breathing: Adults vs. Children
Cheyne-Stokes breathing is predominantly observed in adults, especially those with advanced medical conditions like heart failure or brain injury. In children, this breathing pattern is rare and usually indicative of serious underlying health issues. The presence of Cheyne-Stokes breathing in either group requires prompt medical evaluation and intervention.
Shared Symptoms and Unique Features
Both pediatric and adult OSA share symptoms such as daytime fatigue and recurrent apneas, yet their associated conditions and underlying mechanisms differ:
- Pediatric OSA is more likely to arise from anatomical abnormalities and developmental issues.
- Adult OSA is frequently linked to obesity and comorbidities like Pickwickian syndrome or cardiovascular diseases.
These distinctions underscore the importance of age-specific diagnostic approaches and tailored treatment strategies to manage OSA effectively in both populations.
Overview of ICD-10 Coding System
The International Classification of Diseases, 10th Revision (ICD-10), provides a standardized coding system for diagnosing and documenting medical conditions, including OSA. OSA is classified under code G47.33 in the ICD-10.
This coding system allows healthcare professionals to accurately classify and track the prevalence of OSA across populations.
Moreover, it enables communication among healthcare providers, insurers, and researchers, ensuring consistency in diagnosis and treatment protocols.
Utilizing ICD-10 Codes for Diagnosis
Healthcare providers utilize ICD-10 codes to diagnose OSA based on clinical assessment, polysomnography results, and patient-reported symptoms. During clinical evaluation, physicians assess the presence and severity of symptoms such as daytime sleepiness, snoring, and witnessed apneas.
They consider the patient's medical history, including comorbidities such as hypertension and cardiovascular disease.
Polysomnography (gold standard diagnostic test for OSA) measures various parameters during sleep, including airflow, oxygen saturation, and respiratory effort. Interpreting polysomnography results helps confirm the diagnosis and determine the severity of OSA.
Treatment Options for Obstructive Sleep Apnea
Continuous Positive Airway Pressure (CPAP) Therapy
- Continuous Positive Airway Pressure (CPAP) therapy is the main treatment for adults with moderate to severe obstructive sleep apnea (OSA).
- The procedure involves wearing a mask connected to a machine that delivers a constant air stream, keeping the airway open during sleep.
- CPAP therapy effectively prevents airway collapse and alleviates symptoms such as snoring, daytime sleepiness, and fatigue.
- Compliance with CPAP therapy is crucial for its effectiveness, and adjustments to mask fit and air pressure may be necessary to ensure patient comfort.
- Regular follow-ups with healthcare professionals are essential to check progress and address any issues or concerns regarding CPAP therapy.
✅ Pros:
- Provides immediate and effective airway support, reducing apnea episodes.
- Improves sleep quality and daytime energy levels significantly.
- Non-invasive and widely recommended for moderate to severe sleep apnea.
❌ Cons:
- Some users experience discomfort or difficulty adjusting to the mask.
- Regular maintenance and cleaning are required to prevent infections.
Oral Appliances and Dental Devices
- Oral appliances and dental devices offer an alternative treatment option for patients with mild to mild OSA or those who cannot tolerate CPAP therapy.
- As for Mild sleep apnea, it is a form of sleep apnea where individuals experience 5–15 breathing interruptions per hour during sleep, often causing mild daytime fatigue, snoring, and disrupted sleep quality.
- These devices work by repositioning the lower jaw or tongue to avoid airway blockage during sleep.
- Custom-fit oral appliances prescribed by dentists or sleep specialists provide optimal effectiveness and comfort.
- While oral appliances may effectively reduce symptoms such as snoring and improve sleep quality, they might not be equivalent to CPAP therapy for severe cases of OSA.
- Regular follow-ups with healthcare providers are necessary to monitor the effectiveness of oral appliances and address any issues related to their use.
✅ Pros:
- A comfortable and portable alternative to CPAP therapy.
- Effectively repositions the jaw to reduce airway obstruction.
- Ideal for mild to moderate sleep apnea cases without invasive procedures.
❌ Cons:
- May cause jaw pain or dental misalignment over time.
- Not as effective for severe obstructive sleep apnea cases.
Surgical Interventions and Procedures
- Surgical interventions are considered when conservative treatments such as CPAP therapy and oral appliances fail to manage OSA adequately.
- Surgical options aim to enlarge the upper airway and reduce obstructions, addressing anatomical abnormalities contributing to airway collapse.
- Common surgical procedures for OSA include uvulopalatopharyngoplasty (UPPP), tonsillectomy, adenoidectomy, and maxillomandibular advancement (MMA). A mandibular advancement device is a custom-fitted oral appliance that repositions the lower jaw forward to reduce airway obstruction and treat obstructive sleep apnea.
- Risks and potential complications may accompany surgical interventions, and success rates differ based on the patient's specific anatomy and the severity of OSA.
- Careful evaluation and discussion with healthcare providers are important in determining the most appropriate surgical approach and managing outcomes and recovery expectations.
✅ Pros:
- Provides long-term solutions for anatomical obstructions.
- Reduces or eliminates sleep apnea symptoms for many patients.
- Suitable for those who cannot tolerate CPAP or oral appliances.
❌ Cons:
- Involves surgical risks, including infection and extended recovery time.
- Success rates vary, and some patients may still need additional therapy.
Recent Developments: The FDA recently approved Zepbound (tirzepatide) as a breakthrough medication for treating obstructive sleep apnea in adults with obesity. This advancement offers a promising alternative for patients who struggle with CPAP therapy or other conventional treatment options.
Lifestyle Modifications and Home Remedies
Managing obstructive sleep apnoea (OSA) effectively often involves more than medical interventions. Lifestyle changes and home remedies can significantly enhance the management of symptoms, improve sleep quality, and promote overall well-being. Below are some key strategies to consider.
Weight Management and Dietary Changes
Maintaining a healthy weight is a cornerstone of OSA management. Excess weight, particularly around the neck, can exacerbate airway obstruction during sleep. Weight loss not only reduces the severity of OSA symptoms but also lowers the risk of associated health conditions such as hypertension and diabetes.
Adopting a nutritious diet rich in fruits, vegetables, lean proteins, and whole grains supports weight loss and overall health. Avoiding high-calorie, processed foods and sugary drinks can further aid in managing weight effectively.
Additionally, limiting alcohol and caffeine intake, especially in the evening, can minimize sleep disturbances. Alcohol relaxes the throat muscles, while caffeine can interfere with sleep cycles, both of which can worsen OSA symptoms.
Positional Therapy and Sleep Hygiene Practices
Positional therapy focuses on adjusting sleeping positions to prevent airway obstruction. For individuals with positional OSA, sleeping on the side instead of the back can reduce the frequency of airway collapse. Specialized pillows and positional aids, such as wedge pillows or body pillows, help maintain side-sleeping posture and ensure proper alignment of the head and neck.
Incorporating good sleep hygiene practices is equally essential. Maintaining a consistent sleep schedule, even on weekends, helps regulate the body’s internal clock. Creating a comfortable sleep environment—cool, dark, and quiet—can enhance relaxation and improve sleep quality. Avoiding electronic devices at least an hour before bedtime reduces exposure to blue light, which can disrupt melatonin production and delay sleep onset.
Continuous Positive Airway Pressure (CPAP) Adherence
Continuous Positive Airway Pressure (CPAP) therapy is the gold standard treatment for OSA. The consistent use of CPAP devices prevents airway collapse by delivering a steady stream of air to keep the airway open during sleep. Patients must use CPAP devices nightly as prescribed by their healthcare providers to maximize benefits.
Proper cleaning and maintenance of CPAP equipment are crucial for optimal performance. Dirty or poorly maintained equipment can lead to reduced efficacy and increased risk of respiratory infections. Patients should communicate any discomfort or issues, such as mask fit or air pressure settings, to their healthcare providers. Addressing these concerns promptly ensures the therapy remains effective and comfortable.
Smoking Cessation
Smoking aggravates OSA by inflaming and irritating the airways, leading to increased swelling and mucus production. This narrows the airway, making breathing more difficult during sleep. Quitting smoking not only reduces OSA symptoms but also improves lung health and lowers the risk of cardiovascular complications associated with the condition.
Healthcare providers can offer smoking cessation resources, such as counseling, nicotine replacement therapies, or prescription medications, to support patients in their efforts to quit. A smoke-free lifestyle significantly contributes to better overall health and improved sleep quality.
Avoidance of Sedatives and Alcohol
Sedatives, including certain medications and alcohol, relax the throat muscles, increasing the likelihood of airway obstruction during sleep. Avoiding these substances, especially in the evening, can help maintain muscle tone and reduce OSA severity.
Patients should inform their healthcare providers about all medications they are taking, as some may exacerbate OSA symptoms. Providers can recommend alternatives or adjust dosages to ensure these medications do not interfere with sleep.
Incorporating Regular Exercise
Engaging in regular physical activity is beneficial for OSA management. Exercise helps with weight loss and improves overall cardiovascular and respiratory health, both of which are essential for reducing OSA symptoms. Aerobic exercises, strength training, and activities such as yoga can enhance lung function and promote relaxation, leading to better sleep quality.
Even moderate physical activity, such as brisk walking or cycling, can make a difference. Aim for at least 30 minutes of exercise most days of the week to achieve noticeable improvements in OSA symptoms and overall health.
A Holistic Approach to OSA Management
Lifestyle modifications and home remedies provide a holistic and accessible way to manage OSA effectively. By combining weight management, positional therapy, adherence to CPAP, smoking cessation, and regular exercise, individuals can significantly reduce symptoms and enhance their quality of life. These strategies, alongside medical treatments, empower patients to take an active role in their OSA care and achieve better sleep and overall well-being.

Medications and Pharmacological Treatments
Medications are not typically the primary treatment for obstructive sleep apnea (OSA) but can play a supporting role in managing symptoms or addressing related conditions. Below, we explore the types of medications used, their purposes, and the role of ICD-10 coding in prescription documentation.
Overview of Medications Used in OSA Management
Medications for OSA are generally used to complement primary treatments such as CPAP (Continuous Positive Airway Pressure) therapy or oral appliances. They aim to address specific symptoms or conditions associated with OSA. Commonly prescribed medications include:
- Nasal Decongestants and Steroids
- These medications are effective in reducing nasal congestion and inflammation.
- By improving airflow, they help decrease the severity of OSA symptoms, particularly in patients with nasal obstruction or chronic congestion.
- Nasal sprays or oral decongestants are often recommended for short-term use, especially during allergy season or when congestion is at its peak.
- Oral Appliance Adjuncts
- Patients using oral appliances for OSA treatment may experience side effects like dry mouth or oral irritation.
- Specific medications, such as saliva substitutes or topical gels, can alleviate these symptoms, enhancing comfort and adherence to treatment.
- Medications for Comorbid Conditions
- OSA is frequently linked to conditions like hypertension, cardiovascular disease, and depression.
- Prescribing medications to manage these comorbidities can improve overall health outcomes and complement OSA treatment.
- For instance, antihypertensive drugs can help regulate blood pressure, reducing the cardiovascular risks associated with untreated OSA.
Understanding ICD-10 Coding for Prescriptions
Accurate documentation plays a critical role in the management of OSA, especially when medications are prescribed. The International Classification of Diseases, Tenth Revision (ICD-10), serves as a standardized system for this purpose.
- Purpose of ICD-10 in Prescription Documentation
- ICD-10 codes are used to document medical diagnoses and procedures, including conditions like OSA.
- When prescribing medications, healthcare providers may use specific codes, such as G47.33 (Obstructive Sleep Apnea), to indicate the condition being treated.
- Benefits of ICD-10 Coding
- The coding system ensures accurate documentation of the patient’s medical history and treatment regimen.
- It facilitates clear communication among healthcare providers, enhancing coordinated care for OSA patients.
- Proper coding also supports appropriate insurance reimbursement for prescribed medications, reducing administrative errors and delays.
The Role of Medications in Comprehensive OSA Care
While medications alone are not sufficient to treat OSA, they can enhance symptom management and improve quality of life when used as part of a comprehensive treatment plan. Whether addressing nasal congestion, oral appliance discomfort, or comorbid conditions, pharmacological treatments provide valuable support for individuals managing OSA.
Understanding ICD-10 Coding for Prescriptions
The International Classification of Diseases, Tenth Revision (ICD-10), provides a standardized coding system for documenting medical diagnoses and procedures.
While ICD-10 codes are primarily used for diagnostic purposes, they can also be used in prescription documentation to indicate the medical condition being treated. Healthcare providers may use specific ICD-10 codes related to OSA (such as G47.33) when prescribing medications for OSA management.
This coding system facilitates accurate documentation of the patient's medical history and treatment regimen, streamlines communication among healthcare providers, and ensures appropriate reimbursement for prescribed medications.
Insurance Coverage and Billing Considerations
(Understanding Insurance Policies and Coverage)
Policy Variability and Coverage Limits:
Insurance coverage for obstructive sleep apnea (OSA) treatment varies based on providers, policy types, and specific plan benefits. Patients must comprehend these diverse coverage limits and policy variables to make informed healthcare decisions.
Financial Implications and Patient Responsibilities:
Patients must meticulously review insurance policies and understand copayments, deductibles, and out-of-pocket expenses related to OSA treatment.
Billing Practices and ICD-10 Coding Guidelines
Documentation Standards and Compliance:
Healthcare providers adhere to specific coding guidelines outlined by the International Classification of Diseases, Tenth Revision (ICD-10), to accurately document OSA diagnoses, procedures, and treatments. Compliance with coding standards ensures precise billing practices and supports insurance requirements.
Navigating Coding Changes and Regulations:
Staying updated on evolving coding guidelines and insurance regulations is imperative for billing accuracy. Healthcare professionals must navigate coding changes and regulations efficiently to minimize claim denials and billing errors.
Preauthorization and Prior Authorization Requirements
Navigating Preauthorization Processes:
Understanding preauthorization requirements is crucial for scheduling OSA diagnostic tests and treatments. Patients and healthcare providers must navigate preauthorization processes to ensure timely access to essential healthcare services.
Mitigating Denials and Financial Risks:
Failure to obtain preauthorization or prior authorization can lead to claim denials and financial burdens for patients. Collaboration with insurance representatives and adherence to preauthorization protocols mitigate denials and financial risks associated with OSA treatment.
Patient Education and Support Resources
Managing obstructive sleep apnea (OSA) effectively requires more than medical treatment. Comprehensive care often includes education and building supportive networks. Here are three essential categories of resources to help patients and their families navigate OSA management and improve their quality of life.
Support Groups and Online Communities
- Local Support Groups
- Many communities host in-person support groups tailored for individuals with OSA.
- These groups create opportunities to share experiences, discuss coping strategies, and provide emotional support.
- Participants often find motivation to adhere to treatment plans and build lasting connections with others who understand their journey.
- Online Communities
- Virtual spaces like forums, Facebook groups, and health-specific websites connect individuals across the globe.
- Patients can share personal stories, exchange advice, and access educational resources conveniently from home.
- Online groups foster a sense of belonging and reduce feelings of isolation, especially for those who cannot attend local meetings.
By engaging with support groups—both online and offline—patients can tap into collective wisdom, discover new strategies, and feel less alone in managing their condition.
Educational Materials and Websites
- Sleep Clinics and Centers
- Sleep clinics provide tailored educational resources such as brochures, handouts, and guides focused on OSA.
- These materials address lifestyle modifications, treatment options, and the importance of regular follow-ups.
- Families also benefit from these resources by gaining a better understanding of how to support their loved ones.
- Professional Organizations
- Trusted organizations like the American Academy of Sleep Medicine (AASM) and the American Sleep Apnea Association (ASAA) offer comprehensive online resources.
- Their websites include articles, videos, webinars, and downloadable guides covering OSA diagnosis, treatment, and self-care.
- These resources empower patients with evidence-based knowledge, enabling them to advocate for themselves and make informed health decisions.
Educational materials and websites are valuable tools for fostering understanding and promoting patient autonomy in managing OSA.
Peer Mentorship Programs
- Mentorship Pairing Programs
- Peer mentorship programs, often organized by healthcare providers or advocacy groups, pair newly diagnosed patients with experienced individuals.
- Mentors share practical advice, coping strategies, and encouragement based on their personal experiences managing OSA.
- This peer-to-peer support helps patients feel understood and more confident in navigating their diagnosis.
- Patient Education Workshops
- Workshops conducted by healthcare professionals provide hands-on learning opportunities.
- Common topics include OSA awareness, treatment adherence, lifestyle changes, and coping strategies for better sleep.
- These sessions allow participants to ask questions and receive guidance in a supportive environment.
Peer mentorship and educational workshops bridge the gap between clinical care and real-world application, ensuring patients have the tools and encouragement needed for success.
The Benefits of Comprehensive Support
Combining education and support helps patients manage their condition more effectively. Support groups foster community and shared learning, while online platforms and professional organizations offer access to extensive educational resources. Peer mentorship programs and workshops add a personalized touch, addressing unique challenges and empowering individuals to take charge of their health.
Analysis of ICD-10 Code G47.33 for Obstructive Sleep Apnea (OSA)
1. Overview of ICD-10 Code G47.33
The ICD-10 code G47.33 is the official medical classification for Obstructive Sleep Apnea (OSA). It falls under the broader category G47 (Sleep Disorders) in the International Classification of Diseases, 10th Revision (ICD-10), which is maintained by the World Health Organization (WHO). This specific code is used by healthcare providers, insurance companies, and medical billing professionals to accurately document and classify cases of OSA for diagnosis, treatment, and reimbursement purposes.
2. Clinical Significance of G47.33
- Identifies a Confirmed OSA Diagnosis: The use of G47.33 in medical records indicates that a patient has undergone appropriate diagnostic evaluations, such as a polysomnography (sleep study) or a home sleep apnea test (HSAT), and has been diagnosed with OSA.
- Guides Treatment Decisions: Accurate coding helps in determining the best treatment plan for patients, whether it be CPAP therapy, oral appliances, lifestyle modifications, or surgical interventions.
- Facilitates Research and Public Health Monitoring: By categorizing patients under G47.33, healthcare providers and researchers can track the prevalence of OSA and evaluate trends in treatment effectiveness.
3. Role of G47.33 in Medical Billing and Insurance Claims
- Ensures Proper Reimbursement: Insurance providers, including Medicare and private health insurers, use ICD-10 codes to process claims. Correctly coding OSA with G47.33 ensures that patients receive coverage for diagnostic tests, CPAP machines, BiPAP therapy, or other necessary treatments.
- Reduces Claim Denials: Incorrect or missing ICD-10 codes often lead to insurance claim rejections or delays. Using G47.33 accurately prevents administrative issues that could hinder patient access to treatment.
- Compliance with Healthcare Regulations: Proper ICD-10 coding ensures that healthcare providers adhere to HIPAA regulations, meet payer requirements, and maintain accurate records for audits or compliance checks.
4. Common Secondary Codes Used Alongside G47.33
To capture the full clinical picture, healthcare providers may use additional ICD-10 codes alongside G47.33, including:
- E66.9 (Obesity, unspecified): Many OSA patients have obesity as a contributing factor.
- R06.81 (Apnea, unspecified): Used when apnea is suspected but not yet confirmed.
- J98.8 (Other specified respiratory disorders): Covers additional respiratory conditions that may impact OSA.
5. Why Accurate ICD-10 Coding is Crucial for OSA Management
- Improves patient care coordination by ensuring all providers involved in a patient’s treatment are aware of the condition.
- Helps in securing insurance approval for necessary sleep studies and CPAP devices.
- Supports medical research and epidemiology efforts by providing structured data on OSA trends.
Conclusion
The ICD-10 code G47.33 plays a critical role in diagnosing, treating, and billing for obstructive sleep apnea. Accurate documentation not only streamlines insurance processes but also ensures patients receive timely and appropriate treatment, ultimately improving their quality of life. Healthcare providers must stay updated on coding guidelines to enhance patient outcomes and optimize reimbursement procedures.
CONCLUSION:
The comprehensive treatment options outlined in the Obstructive Sleep Apnea Treatment option offer effective avenues for managing obstructive sleep apnea.
From CPAP therapy to lifestyle modifications, patients have diverse strategies to address their condition.
Individuals can confidently navigate their journey by understanding the importance of treatment adherence and seeking support from healthcare providers.
Empowering patients with knowledge and resources fosters proactive engagement, ultimately enhancing their quality of life and well-being amidst the challenges posed by obstructive sleep apnea.
Frequently Asked Questions:
What's the ICD-10 code for obstructive sleep apnea?
The ICD-10 code for obstructive sleep apnea is G47.33. This alphanumeric code is a standardized classification system healthcare providers use to document medical diagnoses. It allows for consistent coding and facilitates accurate communication among healthcare professionals, insurers, and researchers regarding the diagnosis and the best treatment of obstructive sleep apnea across various healthcare settings and systems.
What does obstructive sleep apnea G47 33 mean?
Obstructive sleep apnea, identified by the ICD-10 code G47.33, is a serious sleep disorder characterized by regular episodes of partial or complete upper airway obstruction during sleep. This obstruction causes pauses in breathing and disrupts normal sleep patterns. Healthcare professionals use G47.33 as a diagnostic code for medical documentation and billing.
What is the ICD-10 code for G47 39?
The ICD-10 code G47.39 corresponds to "other sleep apnea." It encompasses sleep-related breathing disorders beyond obstructive sleep apnea (OSA). This code documents conditions like central or mixed sleep apnea, where breathing pauses during sleep may not solely result from upper airway obstruction. G47.39 aids in accurate diagnosis and medical coding.
What is the ICD-10 code for G47 31?
The ICD-10 code G47.31 corresponds to "primary central sleep apnea." This code documents cases where sleep apnea occurs due to a malfunction in the brain's respiratory control centers. Unlike obstructive sleep apnea (OSA), which involves airway obstruction, primary central sleep apnea is characterized by pauses in breathing without respiratory effort.
DEFINITION OF TECHNICAL TERMS
ICD-10-CM Diagnosis:
Coding system for medical diagnoses; part of the International Classification of Diseases, 10th Revision, Clinical Modification.
Sleep Terrors:
Episodes of intense fear during sleep are often characterized by screaming, thrashing, and a lack of memory of the event.
Cardiac Arrhythmias:
Irregular heart rhythms, including tachycardia, bradycardia, and atrial fibrillation, affect the heart's ability to pump blood effectively.
Conditions Classified Elsewhere:
Medical conditions are listed in one category but more appropriately classified in another according to specific guidelines.
Nonorganic Sleep Disorders:
Sleep disturbances not caused by underlying medical or psychiatric conditions a often related to environmental or behavioral factors.
Frequent Partial Arousals Occur
Repeated episodes of waking partially during sleep, often disrupting sleep continuity—assigned ICD-10-CM code for diagnostic purposes.
REFERENCES
Books:
- Dr. Shiela Ber, Dr. Meir Kryger, and Dr. Michel Guilleminault. Sleep Apnea: The Phantom of the Night. Springer; 2007.
- Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem" edited by Institute of Medicine (US) Committee on Sleep Medicine and Research - National Academies Press; 2006
- W. Chris Winter, M.D. The Sleep Solution: Why Your Sleep is Broken and How to Fix It. - Berkley; 2017.
- Paul Glovinsky, Ph.D., and Art Spielman, Ph.D. The Insomnia Answer: A Personalized Program for Identifying and Overcoming the Three Types of Insomnia. - Avery; 2006.
- Dr. William C. Dement and Christopher Vaughan. The Promise of Sleep: A Pioneer in Sleep Medicine Explores the Vital Connection Between Health, Happiness, and a Good Night's Sleep. - Delacorte Press; 1999.
Websites:
- American Academy of Sleep Medicine (AASM): https://aasm.org/
- National Sleep Foundation: https://www.sleepfoundation.org/
- American Sleep Apnea Association: https://www.sleepapnea.org/
- Mayo Clinic - Sleep Apnea: https://www.mayoclinic.org/diseases-conditions/sleep-apnea/
- WebMD - Sleep Apnea Health Center: https://www.webmd.com/sleep-disorders/sleep-apnea/
- Diagnosis and Management of Obstructive Sleep Apnea– MDPI Journal:This systematic review discusses current diagnostic methods and treatment options for OSA, highlighting areas for improvement in accuracy and cost-effectiveness.